Duration: 2025-2028
Partners: IANPHI, Sante Publique France, Robert Koch Institute, LSHTM, Lancet Countdown, WHO, MCC
Activity Leads: Mathilde Pascale (SPF), Shubhayu Saha (PHI), Angelina Taylor (RKI) Ollie Jay (University of Sydney)
Initiative Background
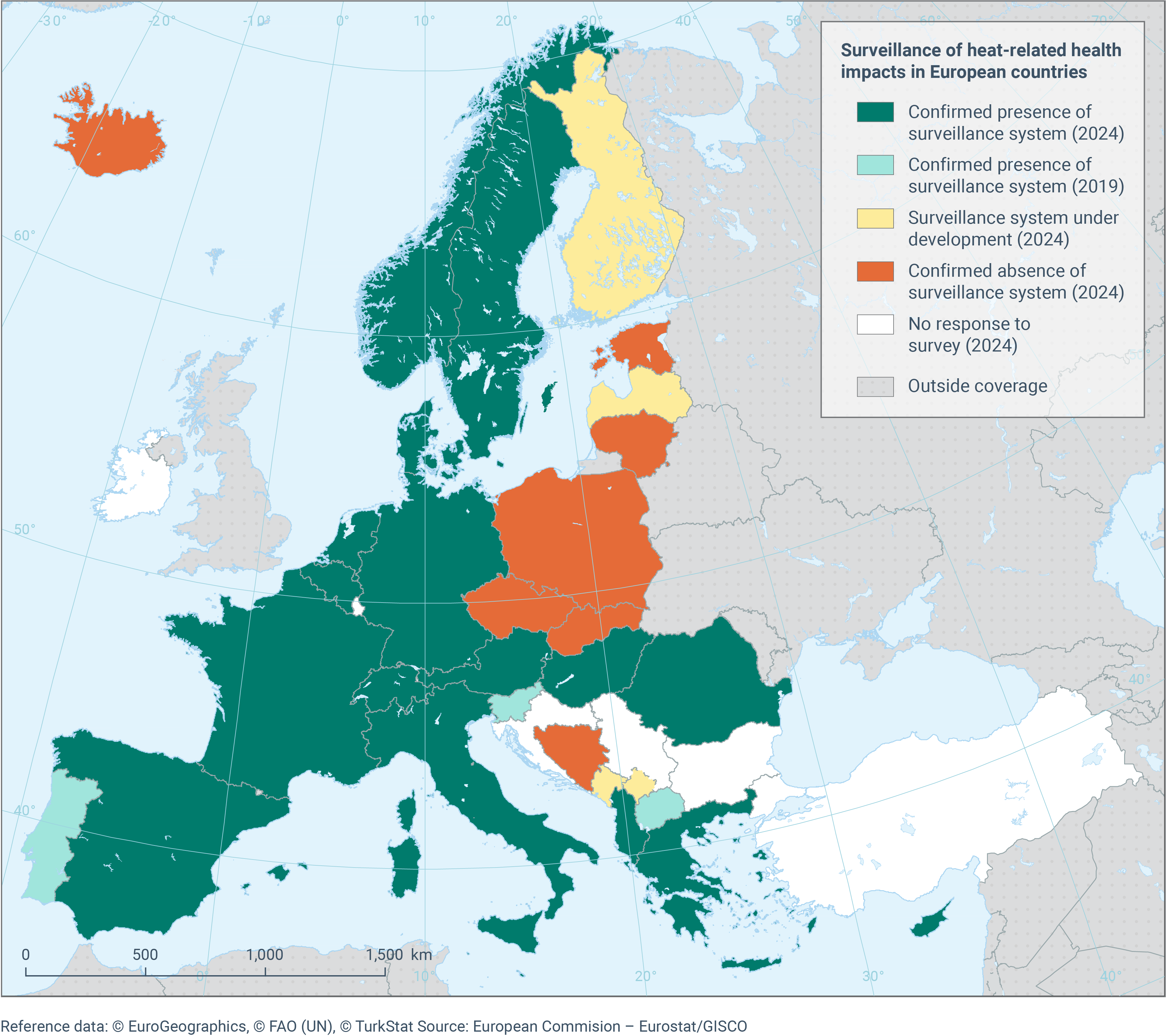
Extreme heat is a growing public health emergency. Estimates of preventable heat-related deaths and heat illness and injury each year vary significantly by geography, from tens to ten of thousands, yet due to differences in methodologies and data collection – the true burden remains unclear, especially in low- and middle-income countries. Today, most countries lack consistent systems to track heat-related illness and death. Existing vital registries, and public health and occupational health surveillance are limited in many countries, fragmented, and varies widely in methods and metrics.
A recent global survey by IANPHI and partners revealed that only a handful of countries estimate heat-related mortality, often using the best available but often inconsistent data sources and definitions. Without standardized approaches to detecting and registering the impacts of heat on health – true burdens are being systematically underreported, leading to gaps in preparedness, poor risk assessments, and missed opportunities to protect the most vulnerable.
A coordinated global effort is urgently needed to map current practices, compare methodologies, and build consensus on core indicators. Strengthening and harmonizing measures will help countries and public health agencies better track risks, understand trends, and inform evidence-based policies to save lives.
This initiative aims to strengthen efforts at global scale to measure and communicate heat-related health impacts, focusing on improving the harmonization and implementation of heat impact registry at national and global levels.
It seeks to encourage the development of more robust, actionable metrics which can effectively communicate and inform emergency preparedness and public health policies and investments, leading to more equitable and evidence-based heat action worldwide.
Main activities
- Assess Current Practices: Review (a) current measures of extreme heat exposure indicators and indices, (b) physiological and clinical indicators of heat stress; c) current heat-health surveillance systems, including coverage, metrics, and estimation methods, in order to identify commonalities, key barriers, enablers, and lessons learned in their implementation.
- Support National and Sub-national Capacity: Identify strategies to strengthen the ability of National Public Health Institutes (NPHIs) to track heat-related mortality and morbidity, both in real time and retrospectively, with disaggregated data and annual estimates. This includes promoting cross-sectoral collaboration with agencies in agriculture, labor, and women’s and children’s health.
- Develop Standardized Indicators: Support the creation of a global monitoring framework by defining core heat-health indicators and providing practical guidance for governments on partnering with meteorological authorities and using surveillance data to inform policies and decisions.
- Build partnerships to advance Global Metrics: Review, prioritize, support, and recommend methods for calculating global-scale indicators of heat exposure and health impacts.
Outputs
- Current global synthesis of heat health surveillance programs and their applications in decision-making.
- Guidance for NMHS and meteorological community to provide more robust heat exposure indicators and indices; for NPHIs to establish/expand heat health surveillance systems and develop standardized heat health metrics.
- Support for peer-to-peer learning in heat health surveillance among countries in different regions of the world by pairing early adopters with those intending to build capacity.
- Utility mapping of real-time and retrospective heat health surveillance information on risk communication, heat action planning and other climate resilience initiatives in non-health sectors like housing, transportation, urban planning and energy.
Aims
- Standardized heat-health indicators are consistently used across global platforms, enabling coherent and comparable global tracking of heat-related health impacts.
- National and subnational surveillance systems develop capacity to measure and track the multiple dimensions of heat impacts on health outcomes and health systems.
- Economic metrics are available for integration into heat-health risk and impact assessments, allowing for the evaluation of the cost-effectiveness and value of heat-risk reduction strategies in public health and climate resilience planning.